Our Research
Clonal dynamics and single cell transcriptomics of luminal epithelial cells in aging and cancer
Age-related prostate diseases are among the most frequently encountered conditions in the male population and age remains a major risk for prostate cancer (PCa) development. Understanding the cellular origins of age-related prostate hyperplasia and dysplasia and finding novel ways to halt progression towards malignancy remain fundamental challenges of PCa treatment, prevention, and patient stratification. Elucidating how aging alters the barriers posed by normal homeostasis to tumor cells expansions is of paramount importance for understanding PCa initiation. To date, it remains elusive how prostate clonal activity maintains the constant prostate size and what homeostatic barriers need to be disrupted for the age-related hyperproliferations to occur and lead to cancer. Moreover, altered aging prostate epithelial cell types and mechanisms that facilitate clonal expansion of tumor cells in aging are not well understood. These unresolved questions hamper the development of anti-proliferative therapies designed to block the deregulated activity of aged prostate epithelial cells. We used in vivo lineage tracing with multicolor reporters, whole organ mapping and single cell transcriptomics to study clonal dynamics of the luminal epithelial layer at single cell resolution. Our ongoing studies address the targetable vulnerabilities in luminal clusters in order to provide new venues for therapeutic interventions against age-related prostate hyperproliferations.
Intratumor heterogeneity and clonal dynamics underlying treatment resistance in prostate cancer
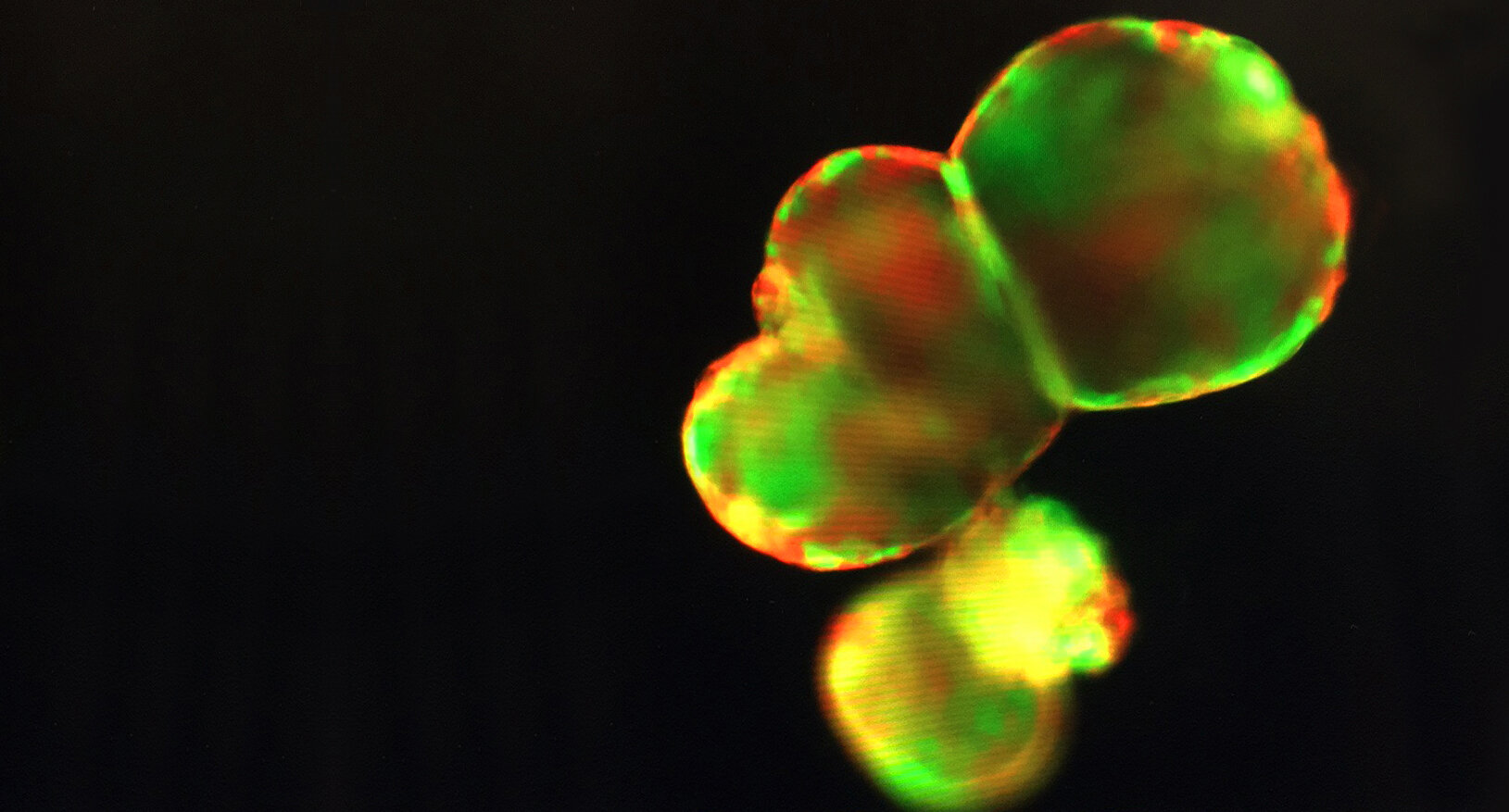
Prostate cancer (PCa) is one of the most common cancers in men worldwide and a leading cause of cancer-related mortality. Though PCa is known to be substantially heterogeneous at the molecular and histological level, there is still little understanding of the tumor subpopulations (“clones”) generating this intratumor heterogeneity (ITH) and their underlying clonal dynamics and interactions. The impact of ITH on disease outcome remains unknown and is thus a significant hurdle in treatment of PCa. This barrier is especially evident in progression to castration resistance: after initial androgen dependence, subpopulations that are castration resistant and less dependent on androgens emerge to populate the tumor, contributing to disease progression. The introduction of second generation androgen deprivation therapies has shown some success in treating castration resistant prostate cancer (CRPC), but eventually drug resistant clones emerge and the disease recurs. Understanding the fundamental differences––both phenotypic and genomic––between clones may hold the key to improving therapies, preventing disease progression, and prolonging patient survival. Using a multi-omics approach, we are exploring the dynamic changes in these subpopulations during progression to castration and drug resistance, focusing on the differences between clones at the transcriptomic and genomic level. Thus far, we have developed a mouse model of ITH in CRPC with the multicolor Confetti reporter, allowing for spatial distinction between different clones. Using single cell sequencing and RNAseq, we have mapped the evolution of early-stage clones post- castration and identified pathways and gene regulatory networks that potentially grant specific clones their castration resistant phenotype. We have extended our system to in vitro 3D organoid cultures to study the evolution of these clones longitudinally during treatment with the antiandrogens enzalutamide and abiraterone, developing a drug resistant in vitro model of CRPC. We are currently using our organoid system to identify novel drug resistance mechanisms in order to target advanced CRPC, which until now has been considered untreatable and lethal. By characterizing clonal dynamics during disease progression, our studies provide new mechanistic insights for identifying pre-existing high-risk clones with drug resistant phenotypes in PCa and uncovering novel therapeutic targets in CRPC. Our work has implications for designing new therapies aimed to control the emergence of advanced disease, preventing CRPC and drug resistance, with the ultimate goal of reducing mortality and improving prognosis.
Direct conversion of fibroblasts to functional bladder urothelium for cancer modelling and regenerative medicine
The urothelium is a highly specialized transitional epithelium lining the bladder that acts as a critical barrier between blood and urine, preventing harmful waste from entering the bloodstream. Diseases of the urothelium, such as interstitial cystitis (IC) and bladder cancer (BCa), are painful and/or life-threatening, clinically costly, and difficult to treat. There is currently no cure for IC, and treatments focus on mitigating symptoms with limited success. BCa has the highest lifetime treatment costs per patient of all cancers and there are currently no targeted therapies for advanced or metastatic disease, due in large part to the lack of reliable mouse and human models for studying the disease. Thus, there is an urgent clinical need for new approaches to investigating and treating diseases of the urothelium. Here we present a novel method for reprogramming fibroblasts into functional urothelial tissue with a two-part goal: first and foremost, to create clinically relevant, genetically engineered models of bladder cancer, and second, to establish a protocol for generating healthy urothelium from patient fibroblasts for autologous transplantation in the case of cystectomy or damaged tissue due to conditions like cystitis or recurrent urinary tract infection (UTI). Our reprogramming method does not rely on induced pluripotent stem cells (iPSCs), thereby bypassing the intermediate pluripotent state of traditional reprogramming, resulting in a faster and more cost-effective protocol. Instead, we engineer induced multipotent epithelial cells by transiently introducing Yamanaka factors in a pro-epithelial culture. We then prime these induced epithelial cells towards bladder differentiation with a cocktail of transcriptional master regulators, identified through bioinformatic analysis of gene regulatory networks in bladder development. We present our urothelial model as both a three-dimensional in vitro culture and as engineered tissue grown in vivo in recombinant murine renal grafts. Our reprogrammed tissue forms a stratified epithelium strikingly histologically similar to murine urothelium and expresses uroplakins, key functional proteins unique to the urothelium. This novel model system will allow researchers to quickly develop and test therapeutic strategies for urothelial disease.
Mechanisms of immune control of intratumor heterogeneity and clonal competition
Intratumor heterogeneity (ITH) and continuous genomic and phenotypic diversification of tumor subpopulations remain major sources of treatment failure in cancer. While the accumulation of mutations has been extensively studied, tumor landscapes remain an unknown geography leaving important non-genetic determinants of ITH unidentified. To uncover the spatial organizational principles of tumor landscapes and cellular networks we propose a “zooming-out” approach through spatial transcriptomics and single cell multiomics followed by “zoom- in” on key regulators of clonal-immune interactions through organoid cultures and in vivo immunomodulatory interventions to steer the tumor landscape towards clonal equilibrium and clonal eradication.